Neuropathic Pain
Neuropathic pain disorders are a set of pain conditions resulting from disorder or injury to the nervous system. The human nervous system is divided into two general parts: the central nervous system, comprising the brain and spinal cord, and the peripheral nervous system, including nerves that go to the limbs, trunk, face and all outlying areas of the body. When nerves of the peripheral system sense pain from mechanical, chemical or thermal sensations, they relay the sensation to the central nervous system for processing. Additionally, the spine and brain command a network a nerves conducting sensation along the back, neck, head and face. Damage to nerves of the peripheral or central nervous system can cause pain signals to be sent to the brain, which may result in the chronic pain condition known as neuropathic pain.
Neuropathic pain may manifest as continuous or episodic, with episodic attacks described as an electric shock and continuous attacks often experienced as feelings of prolonged aching, burning, sensitivity or coldness. Neuropathic orofacial pain conditions refer to those with symptoms that primarily affect a patient’s mouth and face. Orofacial means of the mouth or face.
Trigeminal Neuralgia
The most common orofacial neuropathic pain condition is trigeminal neuralgia, a disorder of the trigeminal or 5th cranial nerve, which causes sudden, severe shock-like pain in or around the face. Episodes typically last several seconds, though they can last up to two minutes, and may repeat in succession and throughout the day.
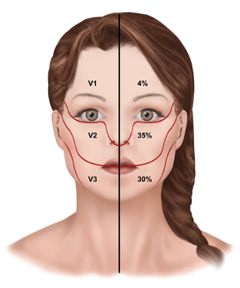
The trigeminal nerve is one of 12 pairs of cranial nerves, the nerves that emerge directly from the brain. The trigeminal nerve has three branches reaching throughout the face and oral cavity. The upper branch is responsible for sensations for the scalp, forehead and front of the head. The middle branch is responsible for sensations in the cheek, upper jaw, top lip, top teeth and gums, and side of the nose. The lower branch is responsible for sensations of the lower jaw, lower teeth and gums, and bottom lip. More than one branch may be affected by a disorder of the nerve, and sufferers may experience pain on both sides of the head and neck, although typically only one side is affected by an episode at a time.

There are other conditions that affect nerves of the central nervous system and cause orofacial neuropathies, such as glossopharyngeal neuralgia, occipital neuralgia, vagal neuralgia and superior laryngeal neuralgia. These orofacial neuropathies are less common, though they are thought to be caused in the same way as trigeminal neuralgia, which is a pressure applied, often by a blood vessel, to the associated nerve as it exits the brain.
An episodic attack of trigeminal neuralgia may be triggered by contact with any of the parts of the face, jaw, mouth and head mentioned above. The condition may become worse over time. Pain may at first be experienced in a small area of the face, later spreading. Episodes can occur for some patients for days, weeks or months and then subside for months or years. If the condition worsens, time between episodes may become shorter and less frequent.
Trigeminal neuralgia has been divided into two types. In Type 1 trigeminal neuralgia, more than half of the pain experienced is shock-like pain described as sudden, sharp, burning or stabbing. In Type 2 trigeminal neuralgia, more than half of the pain experienced is constant pain that is aching, burning or coldness, numbness, or a “pins and needles” sensation. Type 2 trigeminal neuralgia is also known as pre-trigeminal neuralgia as it eventually develops into the classic form of trigeminal neuralgia characterized by intermittent shock episodes.
Atypical Odontalgia
Also among the more common forms of neuropathic orofacial pain is atypical odontalgia. This condition, also known as phantom tooth pain, may follow a dental procedure such as a root canal or an extraction, and is experienced as a pain like a toothache with no actual problem in the tooth.
Oral Nerve Injury
Neuropathy to the inferior alveolar nerve or the lingual nerve occurs most often as a complication of a dental or medical procedure. Tooth extraction, usually of the wisdom teeth, is the leading cause of lingual and inferior alveolar nerve damage. It may also occur as a result of anesthetic injections for oral procedures. The result is pain and burning sensation, numbness or tingling of the tongue, mouth or lower lip.
Complex Regional Pain Syndrome
Complex regional pain syndrome (CRPS), also called causalgia or Reflex Sympathetic Dystrophy Syndrome, is a rare chronic pain condition originating from a disorder of the nervous system. CRPS can affect the craniofacial region, though is more common in the arms and legs. CRPS I is associated with tissue injury and CRPS II is associated with nerve injury. The pain is described as a continuous burning pain and may be accompanied by changes in skin temperature, color and texture, increased skin sensitivity and swelling and stiffness.
Diagnosing Neuropathic Pain
Various orofacial neuropathies derive from a number of causes. Depending on the symptoms experienced, the diagnostic process may be different. For the three most common orofacial neuropathic pain conditions, diagnostic procedures may include the following tests, examinations and considerations.
As with any diagnostic process, a doctor will take a full medical history and description of symptoms, perform a physical exam and any necessary tests or scans.
Trigeminal Neuralgia
Beyond evaluating symptoms, health history and performing a physical exam of the area affected, a doctor may recommend tests to identify medical problems. As with many pain conditions where the exact cause is unknown, trigeminal neuralgia is often diagnosed by eliminating other serious medical problems. A magnetic resonance imaging (MRI) scan may be performed to rule out the presence of a tumor or multiple sclerosis. Rarely, a high-definition magnetic resonance angiography (MRA) may identify where a blood vessel has compressed a nerve. A MRA has been found to detect a vein or artery compressing a nerve in 80 percent of trigeminal neuralgia cases caused by nerve compression. Trigeminal neuralgia may also be positively identified if pain decreases with Tegretol treatment. No single test can reliably identify all cases of trigeminal neuralgia, so diagnosis is dependent on an accurate interpretation of a patient’s signs and symptoms.
Atypical Odontalgia
Diagnosis of atypical neuralgias is difficult and relies on ruling out other possible causes. Along with a clear demonstration of atypical odontalgia symptoms, a doctor may recommend dental X-rays, a MRI or a CT scan to eliminate other possible conditions. Atypical odontalgia, or phantom tooth pain, is often only diagnosed after nerve blocks fail to reduce pain and if test results return no positive diagnoses.
Oral Nerve Injury
Nerve damage is typically diagnosed with one or more of the following tests. An electromyogram (EMG) records the muscle’s electrical activity, with reduced activity suggesting injury to the nerve. A nerve conduction study measures the passing of electrical signals by placing electrodes at two points on the body. And an MRI, or MRA may produce a 3D image of the nerve detailed enough to identify damage.
Complex Regional Pain Syndrome
This complex neuropathic pain condition cannot be diagnosed with a single test, however a number of tests and scans can provide clues to a positive identification. An MRI scan can provide images of changes to tissues. Sympathetic nervous system tests may identify changes to skin temperature, blood flow, sweat or other disturbances to autonomic functions. Changes in bone and blood circulation can be seen with a triple-phase bone scan. An X-ray can identify loss of minerals in bones common in later stages of the condition.
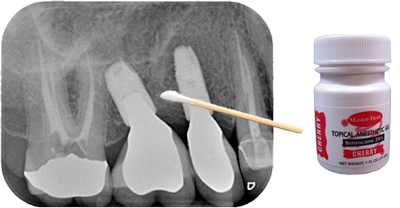
Finding and Blocking a Trigger Zone using a Q-tip Test
When a patient is complaining about pain and the teeth have been ruled out as a cause, the dentist should see if he/she can find the trigger zone and replicate the pain using a Q-tip. First, ask the patient to describe where the pain is occurring and, even better, give them a Q-tip to show you where they are feeling pain. Then using a very light touch with the Q-tip, try stroking the tissue around the area where the patient is reporting their pain and ask them if that hurts. Then try pressing on the same area with firm pressure in various different spots and ask them if that hurts. If you are able to replicate the pain using either of these techniques then the next step is to see if you can reduce or block the pain. Apply a topical anesthetic to the area where you caused the pain with a Q-tip. Wait a few minutes and repeat the Q-tip test to see if you can replicate the pain. Next, try infiltrating the papilla or local tissue where you were able to replicate the pain and repeat the Q-tip test. Last, try blocking the tooth as if you were going to do a restoration and repeat the Q-tip test. If you have ruled out an odontogenic cause of the pain, and any of these methods greatly reduce or block the pain, then it is likely a neuropathic pain of the trigeminal nerve. If you cannot block any of the pain, then the pain is centralized. The next step, especially in the case of pain on the maxillary arch, is to try is a sphenopalatine ganglion block (SPG). This can be done in the office. I use a Sphenocath with 2 cc’s of 4% lidocaine into the nostril on the ipsilateral side of the pain. If you can block the pain using an SPG block, repeat the procedure once a week for a total of six weeks. This will hopefully provide the patient with pain relief for six months or longer.
An important piece of this pain puzzle to keep in mind is if the pain started on its own or if the pain started after a dental procedure or any trauma. If it started on its own, is intermittent, and is described as a sharp, shooting, electrical pain then it is likely trigeminal neuralgia, which can be treated with anti-seizure medications and an MRI must be ordered. If the pain started after a dental procedure, you have ruled out the tooth, is described as a painful, sharp, shooting and/or burning pain that does not go away, and you can reduce the pain or completely block it, then it is likely a post-traumatic trigeminal neuropathic pain (PTNP), which can be treated topically.
MRI Prescription for Trigeminal Neuralgia
This is my MRI prescription for the radiologist:
High resolution MRI with and without contrast of the brain and brain stem with thin cuts through the posterior cranial fossa with attention to the trigeminal nerve using Fiesta images with vascular loop protocol. Rule out space containing lesions, multiple sclerosis, acoustic neuroma, trigeminal neuralgia, etc. Please rule out contact of the superior cerebellar and anterior inferior cerebellar arteries with the trigeminal nerve.
Technical Terms
Allodynia – a painful response to a non-painful stimulus. A great example is skin that has a sunburn, which is painful to the touch. Skin does not normally hurt.
Ephaptic transmission – when light touch triggers pain, the A-beta fibers have undergone a transformation from sending a non-painful signal to a painful signal.
Dynamic mechanical allodynia – pain with light touch.
Static mechanical allodynia – pain with firm pressure.
A-beta fibers – responsible for the sensation of touch. The fibers are myelinated.
A-delta fibers – responsible for the sensation of pain from mechanical and thermal inputs. The fibers are myelinated. These are the “fast pain” fibers such as what you feel when you stick your finger over a fire.
C fibers – responsible for the sensation of pain from mechanical, thermal, and chemical inputs. The fibers are unmyelinated. These are the ” slow pain” fibers, which are what cause pain that lingers.
Life with Neuropathic Pain
Regardless of the specific condition, coping with the painful symptoms of orofacial neuropathies can be a difficult and stressful experience. These little understood conditions pose an added challenge as the uncertainty regarding the cause of the pain can make a sufferer feel a loss of control or helplessness.
Furthermore, the debilitating pain of a neuropathic disorder may prevent a patient from participating in enjoyable activities. As a result, it’s not uncommon that depression and anxiety develop in individuals with chronic neuropathic pain conditions.
Efforts can be made to reduce pain symptoms and maintain a level of normal activity. Relaxation techniques, meditation and engaging in enjoyable hobbies and activities that a patient is able to do may offer some relief from psychological stresses. By continuing to do normal daily activities as able while allowing oneself needed rest, a neuropathic pain patient can continue to feel in control of his or her life.
One suffering from a chronic neuropathic condition may also find mental relief by maintaining an active treatment regimen, including taking prescribed medications, performing physical therapy exercises and following other recommendations from a healthcare professional.
A mental health professional may also be able to help a patient manage feelings of anger or frustration caused by the condition. Support groups for sufferers can offer a community that can relate to the challenges posed by the condition, sharing advice for pain management and support based in personal experience and understanding. The Facial Pain Association is a support group for trigeminal neuralgia patients. Those with CRPS may find support in various groups such as American RSDHope. The National Pain Foundation has online forums and support groups for chronic pain sufferers.
Treatment of Neuropathic Pain
Fortunately for those suffering from facial neuropathies, while much is unknown about causes, a number of treatments have been found effective. A combination of treatments and therapies is often found most effective in managing orofacial neuropathic pain symptoms. As with all neuropathic pain conditions, treatment plans for those disorders discussed here should be developed with the consultation of a doctor.
Trigeminal Neuralgia
- Anti-seizure medications: Medicines that block nerve firing are typically the first line of treatment for trigeminal neuralgia. A doctor may prescribe anticonvulsant drugs including carbamazepine, oxcarbazepine, clonazepam, topiramate and a number of other medications found effective in decreasing nerve overactivity. Proper dosing of these potent medications is often identified by prescribing gradually increasing amounts of the drug and carefully monitoring effects and side effects.
- Tricyclic antidepressants: If pain manifests as constant, burning or aching, tricyclic antidepressants have been found useful in pain management.
- Rhizotomy procedures: Rhizotomy procedures block pain by destroying select nerve fibers. The end result can cause numbness in the face. In the treatment of trigeminal neuralgia, several forms of rhizotomy have been used effectively. Balloon compression blocks pain signals by inflating a balloon next to the trigeminal nerve at the base of the skull with enough pressure to damage the nerve. Radiofrequency lesioning uses electrical currents to identify the portion of the trigeminal nerve responsible for pain and destroys those nerve fibers with a heated electrode. In stereotactic radiosurgery, highly focused beams of radiation directed at the trigeminal nerve at the base of the skull slowly cause a lesion on the nerve over a period of several months.
- Microvascular decompression: This surgical procedure works by implanting a cushion between the trigeminal nerve and the compressing blood vessel.
Atypical Odontalgia
Local anesthetics and steroid injections may reduce pain symptoms if pain originates in a nerve near the teeth or gums. The application of prepared medicinal creams has also been found to provide pain relief. Drug treatment options include antiseizure medications, tricyclic antidepressants or narcotics*.
Oral Nerve Injury
If pain from nerve damage sustained during a dental procedure does not improve within 6 to 8 weeks, surgical repair can be performed. When done within 10 to 12 weeks of the injury, 70 percent of patients report at least a 75 percent improvement of symptoms. The rate of success in repairing injuries to nerves sustained by trauma from dental and medical procedures improves the closer they are performed to the incident.
Complex Regional Pain Syndrome
Treatment for this condition usually consists of a combination of therapies. Medications used to treat CRPS include antidepressants, pain medications and blood pressure medications. A series of injections of anesthetics in main intersections of affected nerves may stem the advancement of the condition if done in the early stages of the disorder. Physical therapy may also be helpful in improving function in, restoring motion of or desensitizing the affected area. As a last resort, sympathectomy, an interruption of the affected portion of the sympathetic nervous system, can be performed by surgical, chemical or radiofrequency means.
* I do not prescribe narcotics for any patient for any reason.
Groups at Risk for Neuropathic Pain
There are a variety of risk factors that can increase the likelihood of developing a neuropathic pain condition. However, as the underlying cause of many neuropathic pain conditions is unknown, there remains considerable uncertainty as to what may increase the incidence of orofacial neuropathy. For the major orofacial neuropathic pain conditions discussed here, some link has been found for the following groups.
Trigeminal neuralgia: This rare condition manifests in approximately 150 per million people every year. Women are more likely than men to suffer from trigeminal neuralgia, and the disorder most often affects those over 50 years old. There may be a genetic link as some evidence suggests that the condition runs in families. The reason for this may be an inherited blood vessel formation prone to nerve compression.
Atypical odontalgia: Little is known about the mechanisms underlying this condition, and in many patients a cause may not be identified. However, one study of patients suffering from phantom tooth pain suggests a connection between atypical odontalgia and migraine headaches and cluster headaches. Those with a personal and family history of idiopathic, or unknown, headache had an increased likelihood of experiencing phantom tooth pain.
Oral nerve injury: An undesirable result of dental procedures, injury to the nerves running along the lower jaw is more likely to occur in individuals requiring procedures such as tooth extraction, local anesthetic or improper implant placement. In one study, lingual nerve damage due to local anesthetic injection was found to manifest in 1 in every 26,000 to 160,000 incidences of injection. Another study found that 0.15% of cases of local aesthetic injections damaged the patient’s lingual nerve, and that after a period of 6 months, symptoms were still present for 0.008% of patients.
Complex regional pain syndrome: While it is thought that CRPS is more common in young women, this neuropathic pain condition affects men and women of all ages. Little is known about the onset of CRPS and underlying causes of the disorder.
Causes of Neuropathic Pain
Neuropathic pain, specifically conditions affecting the head and neck, may result from various of injuries, illness or disorder.
Common causes of trigeminal neuralgia include:
- Nerve compression: Trigeminal neuralgia, the most common neuropathic pain condition, results from disorder of the trigeminal nerve. It is believed that the most common cause of this condition is a blood vessel pressing on the nerve, wearing away at the nerve’s protective coating known as the myelin sheath. Damage done by compression of the nerve can result in deterioration of function whereby abnormal signals are sent to the brain.
- Tumors: A tumor pressing against a nerve may cause deterioration of the myelin sheath. A tumor at the base of the brain may affect the trigeminal nerve, causing pain in the head, neck and face.
- Multiple sclerosis: This auto-immune disease affects the central nervous system, causing inflammation and permanent damage to the myelin sheath of nerves of the brain and spinal cord. The myelin sheath is like insulation for the nerve, and if this insulation is damaged, the nerve can cause severe pain in the head, neck and face as part of a broad spectrum of signs and symptoms.
- Physical injury: An accident or other cause of injury can damage nerves so that they relay messages of pain to the brain. A damaged nerve can continue to refer pain signals to the brain even after an injury is otherwise healed. Common causes of injury to the trigeminal nerve include dental or surgical procedures, infection in the oral cavity and injury to the face.
The cause of atypical odontalgia is unknown, though the condition may be a result of nerve deafferentation, which is the interruption or elimination of nerve fibers. This theory is supported by atypical odontalgia patients where onset of the condition occurs following a dental procedure such as a root canal or extraction. However, there are cases of atypical odontalgia where no procedure has been performed and no known cause identified.
Oral nerve injury is a common complication of dental procedures including extraction of the third molar, also known as the wisdom tooth. It can also occur as a result of an injection of local anesthetic for procedures including fillings, crowns and root canals. Incorrect implant placement may also damage the inferior alveolar or lingual nerve. This damage to these nerves running along the lower jaw can cause pain, tingling or numbness in the tongue, mouth and lower lip.
Complex regional pain syndrome (CRPS) is thought to originate by an injury to tissue or nerves and then perpetuated by irregular behavior in the sympathetic nervous system, a component of the autonomic nervous system responsible mainly for mobilizing the body’s resources under stress and triggering the fight-or-flight response.
Recent research suggests that in cases of CRPS, when an injury to tissue or nerve is sustained, an unknown mechanism results in the sympathetic nervous system maintaining active pain pathways. Another theory suggests that CRPS may be a disruption of the healing response whereby an injury triggers an immune response resulting in inflammation, redness and swelling. More than likely, CRPS is the result of multiple causes occurring at once.
History of Neuropathic Pain
Neuropathic pain conditions have a long history of misdiagnosis as mechanisms are complex, often dependent on multiple factors, and are the result of causes that remain unclear. The healthcare establishment frequently dismissed some orofacial neuropathies as psychosomatic, or imagined conditions originating in the mind.
Atypical odontalgia, or phantom tooth pain, is an example of a condition that was often thought to be imagined pain. The mainstream healthcare community did not recognize phantom pain symptoms until the 1940’s.
Complex regional pain syndrome has previously been known by the names “reflex sympathetic dystrophy syndrome” and “causalgia.” During the Civil War, “causalgia” was coined describe the pain felt by war veterans long after wounds had healed.
Trigeminal neuralgia, a common orofacial neuropathic pain condition, has been recognized in medical literature dating back to the first century A.D. in the writings of ancient Greek physician Aretaeus. However, without an adequate understanding of the mechanisms behind the condition, early treatments included the application of poisons like arsenic, hemlock and animal venom. Nicolaus Andre, an 18th century French surgeon, coined the term “tic douloureux” to describe the condition. The phrase translates as “painful spasm.” Other common neuropathies that affect the orofacial region have a much more recent history of recognition and research. The first medication to treat trigeminal neuralgia was not discovered until the 1940’s.
Today, the National Institutes of Health conduct research into neuropathic pain conditions through its National Institute of Neurological Disorders and Stroke (NINDS). Through this national government organization, biomedical research of disorders of the nervous system and brain are uncovering insights into the mechanisms that cause and perpetuate chronic neuropathic pain. Better medical and surgical treatments for nerve pain disorders are a major goal of studies and research.