Headaches: What You Need to Know
A headache is an ache or pain occurring anywhere in the face, neck or head. Headache pain, whether you live in Beverly Hills, Los Angeles, or anywhere in the world, is experienced through pain-sensitive structures around the head and neck including blood vessels, nerves, muscles and tissues including the eyes, ears and sinuses. Headaches can range across the intensity spectrum from mild, tolerable pain to severe pain that prohibits daily activities. Headaches are one of the most commonly experienced causes of pain. They can be occasional, recurrent or chronic in frequency.
The International Classification of Headache Disorders (ICHD) is published by the International Headache Society to classify and diagnose types of headaches. According to this classification system, there are four primary types of headaches: migraines, tension-type headaches, cluster headaches and other headaches sensed in the cranial nerves. Different types of headaches may respond to different types of treatments as they originate by various causes.
Migraine
A migraine is a moderate to severe headache often accompanied by nausea, vomiting, increased sensitivity to sound, and increased sensitivity to light. The severity, duration and frequency of migraine pain vary from one attack to another in the same person.
There are four possible phases of a migraine, and all are not necessarily experienced. The first phase, called the prodrome, may occur hours or days before the migraine, and consists of an altered mood excessively sleepiness, stiff muscles and other symptoms. The second phase, called an aura, which may immediately precede the attack, occurs in 20 to 30 percent of migraine sufferers. An aura can be motor or sensory, including a disturbance of vision such as flashes of light or zigzag lines, or a feeling of pins and needles in the hand, arm, face and mouth. The third phase of a migraine is the pain or headache phase. The pain may occur on one side of the head or both and usually lasts from 4 hours to 3 days. The final phase of a migraine, a postdrome, may occur for some patients. It may include a sore feeling where the migraine pain was accompanied by feelings of tiredness, weakness and cognitive difficulties. Six percent of men and 18 percent of women are estimated to experience a migraine headache in their lifetime.
Tension-type headaches
These are the most commonly occurring type of primary headache. Up to nine out of ten adults will have or have had a tension-type headache in their lifetime. A tension-type headache is experienced as pain of varying intensity in the head, face and neck, often described as a feeling of tightness or pressure.
Cluster headaches
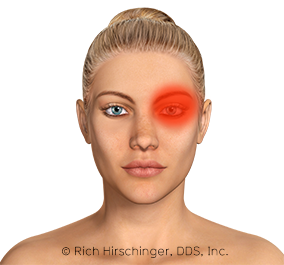
This rare primary headache type only effects 0.1% of the population, most commonly men in their late 20’s. The piercing pain is felt in the eye region, typically on only one side of the face without changing sides. A cluster headache usually lasts between 30 and 90 minutes, but can occur for up to three hours. They are often recurrent, happening regularly at the same time of day or night. Many people who suffer from cluster headaches report between one to three headaches per day during a period.
If you suffer from frequent headaches, finding out the type of headache causing the majority of symptoms is a critical part of treating the underlying causes of the pain. Learn about the major causes, symptoms and treatments for various headache types here, and consult Dr. Hirschinger before starting a treatment plan.
Headache Fact Sheet

According to this classification system established by the International Headache Society in the International Classification of Headache Disorders, there are four primary types of headaches: migraines, tension-type headaches, cluster headaches and other primary headaces.
A tension-type headache is the most common type of primary headache. It is experienced as mild to moderate pain in the head or neck.
A migraine is a moderate to severe headache often accompanied by sensitivity to light and sound, nausea, vomiting and weakness. Six percent of men and 18 percent of women are thought to experience a migraine headache during their lifetime. A migraine may display in up to four stages, the prodrome, the aura, the headache and the postdrome.
A cluster headache is a rare headache type most often experienced by men in their 20’s. It is felt as a piercing pain, usually behind the eye on only one side of the face. Cluster headaches typically occur at the same time each day over a period of weeks or months, followed by a period of regression during which no headaches are experienced for up to a year or more.
A women’s migraines can actually decrease during pregnancy especially in the 2nd and 3rd trimester.
The treatment of a headache varies based on the type of headache. Tension-type headaches may respond to over-the-counter painkillers including aspirin, ibuprofen, acetaminophen and naproxen.
Migraines are often treated with over-the-counter painkillers including aspirin, ibuprofen, acetaminophen and naproxen, or with prescribed medications such as a triptan. Cluster headaches may be relieved by triptans or with oxygen inhalation. Frequent migraine and cluster headache sufferers may also consider treatment plans that prevent the onset of headaches.
Factors that contribute to increased risk of headaches include: obesity, smoking, drinking alcohol, too much or too little physical exertion, and stress.
In order to diagnose and treat a headache, it can be helpful to a doctor if the patient keeps a record of headache incidences. The record should include the length, day and time of the headache, any food or drink that was taken prior to the headache, any activity underwent before the headache, and what, if anything, helped alleviate the pain.
The underlying cause of headaches is largely unknown, however research has revealed some information about the cause and mechanism of headaches. Common migraine triggers include stress, hunger and fatigue. Tension-type headaches can occur as a response to injury, stress or other activity that requires tension in the head and neck. Some research suggests that the cause of cluster headaches can be traced to abnormal activity in the hypothalamus, the region of the brain responsible for the biological clock.
A headache patient may be able to lessen his or her risk for headaches or lessen the frequency, duration or severity of headache pain by making lifestyle changes. Some of these changes include: reducing stress, improving sleep habits, losing excess weight, decreasing smoking or alcohol intake and improving posture or ergonomics if spending long periods at a desk or driving or in other uncomfortable positions.
Diagnosing Headaches

As with all medical conditions, a doctor should be consulted for the proper diagnosis of a headache type. Depending on the type of headache, treatment may differ. Accurate diagnosis of frequent or recurring headaches is critical to finding relief when symptoms occur and establishing both a short-term and long-term treatment plan. Additionally, a headache may be a symptom of an underlying health problem requiring medical attention. In diagnosing headache types, a complete and accurate history of symptoms and characteristics of the headache is helpful. A doctor may ask for information about how the headache feels and characteristics of the headaches, including:
- Describe the type of pain and where it is located.
- What is the severity of the pain on a scale of 1 to 10?
- How long does the pain last?
- How often do headaches occur?
- Have you noticed a trigger, such as situations, food, activities or medicines preempting the headache?
- What symptoms occur along with the headache, such as sensitivity to light and/or sound, nausea, or weakness?
- Does anyone else in your family have headaches?
- When did you first experience this type of headache?
- Do you experience headaches that feel different, or do you have different types of headaches?
In diagnosing a headache patient, a physical or neurological examination may also be conducted to find signs of an underlying cause, such as:
- Trouble with balance
- Vision abnormalities
- High blood pressure
- Fatigue or muscle weakness
- Injuries or head trauma
- Infections
- Malformation
- Tumor
- Hemorrhage
A doctor to aid in the diagnosis of headaches and to rule out or confirm possible causes sometimes uses diagnostic tests such as an MRI. An MRI, which stands for magnetic resonance imaging, of the brain produces images that enable a radiologist to see the soft tissues inside the skull, which might help explain the cause of the headache. Similarly, a CT scan of the head may be ordered. A CT scan, which stands for computed tomography, of the head produces cross-section images of the hard structures of the brain such as the bone. A blood or urine analysis can be used to test for diabetes, thyroid problems or infections along with other medical conditions that can cause headaches.
There are multiple types of headaches and many possible headache causes. Most headache patients will not require an array of extensive diagnostic testing prior to establishing a treatment plan.
Treatments for Headaches
The type and cause of the headache must first be determined before proper treatment can be established. However, there are several headache treatments that relieve symptoms for a variety of headache causes.
Migraine

Migraines can be treated on two fronts: preventive and abortive. Preventive medications seek to avoid the occurrence of a migraine, while abortive medications relieve pain after onset. If a patient suffers from recurring migraines, preventive medications may be considered as part of a treatment plan. Preventive medications usually don’t eliminate headaches completely, but they can help reduce the severity, length and frequency of migraines. Beta-blockers, anti-seizure medications, tricyclic antidepressants, Botox, and CGRP antagonists such as Aimovig, Ajovy, and Emgality have all been found to be potentially effective in preventing the occurrence of migraines in frequent sufferers. Calcium channel blockers are an option, but they are usually tried last since their effectiveness is not as good as the other preventatives. If a moderate migraine is underway, a sufferer may find relief from some over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) such as Aleve, or a combination of aspirin and a cola with caffeine. Severe migraines are more effectively treated with triptans for relief of pain, nausea and/or light and sound sensitivity. Dr. Hirschinger can prescribe triptans, such as sumatriptan, rizatriptan and naratriptan among others, as well as dihydroergotamine (DHE), Nurtec, and Ubrelvy to abort a migraine that has already started.
Tension-type headaches

As tension-type headaches are caused by built up muscle tension in the neck or scalp, a massage may offer some initial pain relief. Over-the-counter pain medications such as aspirin, ibuprofen, acetaminophen, and naproxen can offer effective relief as well. A hot shower or bath or heating pad may also help loosen the muscle tightness causing the pain. Caffeine may also help to relieve tension-type headache pain by dilating blood vessels and increasing blood circulation to the affected muscle region. Treatment options that Dr. Hirschinger may prescribe include muscle relaxants, certain antidepressants, ethyl chloride, trigger point injections, and Botox. Lifestyle changes can be adopted to help with the prevention of headaches in the future, including changing sleep habits, increased exercise and stretching the neck, back and shoulder muscles if long periods of time at a desk or computer are a required part of a headache sufferer’s job or lifestyle, as well as stretching the closing muscles of the jaw, which, when overused, can referred pain into the temples. Dr. Hirschinger is the inventor of the gentle jaw, which helps stretch the closing muscles of the jaw. It is critically important that patients keep their teeth apart during the day since if the teeth are held together, this can and will lead to increased pain and increased tension-type headaches.
Cluster headaches
Unlike other types of headaches, common over-the-counter pain relievers do not typically help abort a cluster headache. Instead, cluster headaches may be relieved by triptans, including sumatriptan, zolmitriptan, and frovatriptan, narcotics (which are frequently avoided as they are habit forming) and pure oxygen. Pain relief from inhaling 100 percent oxygen can be felt within 15 minutes, however this treatment is most effective before pain reaches its peak, so cluster headache patients may need to have an oxygen cylinder and regulator easily available and accessible. Triptans can be administered in an injectable form or nasal spray as an effective treatment for acute cluster headaches. Preventive strategies for cluster headaches include calcium channel blockers, corticosteroids, ergots, melatonin, or antiseizure medications.
Scibabe Interview of Dr. Hirschinger
On August 21, 2020, Dr. Hirschinger was the guest of Yvette, aka Scibabe, for a two hour Question and Answer about primary headaches. Yvette suffered with a 9.5 year headache that was never properly diagnosed. Yes, that does say “year.” Based on the history of the headache that Yvette reported was one sided, and caused her eye to drop, Dr. Hirschinger diagnosed her with hemicrania continua, which is one of the trigeminal autonomic cephalalgias. Hemicrania continue is one of two headaches that is “absolutely responsive” to a certain medication named indomethacin. The other is paroxysmal hemicrania. If the diagnosis is correct, and the patient is placed on a therapeutic dose of indomethacin, the headache must resolve completely. A therapeutic dose of indomethacin is 50 mg three times a day. Yvette was already taking indomethacin but she was only taking 75 mg PRN, which means “as needed.” Dr. Hirschinger had Yvette take 50 mg every 8 hours, and her headache disappeared after five days.
SciBabe Weekly Q&A with special guest Dr. Rich Hirschinger https://t.co/66BpCecZCm
— Yvette, exiled Queen of the Seychelles. (@TheSciBabe) August 22, 2020Reference International Headache Society Trigeminal Autonomic Cephalalgias Hemicrania Continua
Life with Headaches

Sufferers of frequent headaches can often minimize the pain in their lives associated with headaches through a combination of treatment factors. They may find it helpful to manage their pain and prevent symptoms through the use of medications for abortive and preventive relief and the help of a doctor or other sources of reliable treatment education.
It often helps the doctor determine the causes of recurring headaches if a headache sufferer keeps a record of his or her headaches. This includes noting what day and time the pain begins, the last thing a patient ate or drank, recent sleep patterns and any activities that could have contributed to stress or tension. The headache patient should also make note of the duration of the headache and what contributed to making the pain stop, if anything.
In order to alleviate the causal factors of headaches, a headache sufferer should reduce the number of risk factors present. This may include quitting smoking, drinking less or eliminating alcohol, increasing exercise, weight loss, and improving posture at a desk, in a car or other long-held positions. A chronic headache sufferer may also improve headache symptoms by improving sleeping habits, usually by getting more sleep, or reducing lifestyle stressors that may trigger headaches.
Depending on the type and cause of a headache, a person may reduce the frequency, severity and length of headaches by practicing preventive treatments, including medications that can be prescribed by a doctor. Living with headache pain can be a debilitating condition that hinders a person from regular activities of work and recreation. However, the condition may be improved by executing a preventive treatment plan and aggressive relief of pain symptoms once they occur. Understanding why headaches are occurring and obtaining healthcare advice and treatment from a doctor are early steps for effectively reducing the painful symptoms of headache attacks.
History of Headaches
Humans have experienced headaches since ancient times. It is likely that ancient peoples believed that headaches were a sign of evil spirits, and evidence of ancient remedies to relieve what is thought to be headache pain can be traced back as early as 7000 BC. Trepanation, drilling a hole or removing a section of the skull, can be seen in Neolithic skeletal remains and is thought to be a procedure meant to release the demon causing headaches and disorders including epilepsy.

An ancient Egyptian papyrus document, the Ebers Papyrus, dates back to 1200 BC and outlines a ritual for relieving migraines and head pain. In 400 BC, Greek physician Hippocrates recorded symptoms common of a migraine, including visual distortion and intense pain that begins in the temples and gradually radiates throughout the head and neck.
Following the scientific revolution of the 16th century, medical literature recorded observations and treatments of headaches. Considered the founder of clinical neuroscience, Thomas Willis made accurate observations of migraines, introduced the term “neurology,” and was the first to propose that migraine pain was caused by dilation of blood vessels. Erasmus Darwin again supported the vascular theory of headache pain in the 18th century. He found that putting a headache patient in a centrifuge to force blood from the head to the feet offered effective relief from headache pain.
The first major treatise about migraines was published in 1873 by Edward Liveing, however Liveing’s theory explaining the cause of headaches differed from the accepted theory of vasodilation, instead pointing to an overactive central nervous system and “nerve storms.” In the late 19th century, Sir William Gowers, considered a founder of modern neurology, was among the first to divide headache treatments into preventive and abortive. The first to study headaches in a modern laboratory setting was Harold Wolffe during the 1930s. His experiments provided further support that the cause of headache can be traced back to vascular dilation.
The causes and treatment of headaches continue to be an active area of scientific research. Much current research seeks to understand the underlying causes of headaches, brain mechanisms of headaches, social, racial and psychiatric factors that may relate to headaches, and genetic predispositions for headaches. There are also many ongoing clinical studies seeking to relieve and manage headache pain.
Signs and Symptoms of Headaches
Headache symptoms vary by individual, cause, and type. The following are common symptoms of tension-type headaches, migraines and cluster headaches that may be helpful in understanding the pain and accompanying signs being experienced.
Migraines:
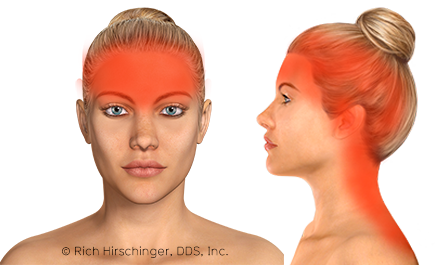
There are several stages that may or may not be experienced as part of a migraine attack. Symptoms of the prodrome, a warning stage that precedes the intense pain of a migraine headache in an estimated 50 percent of cases, include an altered mood and excessive fatigue, yawning and sleepiness. Depression and irritability may also be experienced during this stage. The following stage, which does not always occur, is the aura, which is experienced in 20 percent of cases and can also occur along with the pain. The aura is marked by visual symptoms including flashing lights, a zigzag pattern or a blind spot. The pain or headache stage of a migraine is often described by sufferers as intense, pounding or throbbing pain felt in the temples, forehead, around the eye or back of the neck or head. The pain is usually felt on one side of the head, though may be present on both sides. During this stage of a migraine, a person will frequently also experience nausea, vomiting, sensitivity to light and/or sound, and diarrhea. A migraine attack typically lasts between several hours to several days. Weakness, sleepiness and pain in the area where the headache occurred are symptoms associated with the postdrome, the final stage of a migraine.
Tension-type headaches:
This most common type of headache is marked by mild to moderate pain in the head or neck. A tension-type headache can also cause symptoms of aching muscles as well as sensitivity to light or sound. The pain can cause irritability in the headache sufferer and an inability to concentrate. It may also make it hard to fall asleep or stay asleep, possibly resulting in fatigue. Tension-type headaches may present periodically, daily or recurring more than once per day. Chronic tension-type headaches are experienced as a constantly present pain that varies in severity throughout the day. Tension-type headaches typically respond well to over-the-counter pain relief medications such as aspirin, ibuprofen, acetaminophen, and naproxen.
Cluster headaches:
The term “cluster” refers to the fact that this type of headache manifests in a number of headaches that occur periodically followed by a period of remission. Cluster headaches may occur daily for days, weeks or months, usually during the same time each day, followed by a period of time without headaches. The pain is severe, comes on suddenly and quickly worsens, peaking in about 5 to 10 minutes of onset. The pain is often described as sharp, burning, intense and steady, and almost always occurs on one side of the head, often behind the eye, in the temple, sometimes radiating to the nose or down the neck or shoulder. The time of day a cluster headache occurs is usually a few hours after an individual has fallen asleep, although they may occur during daytime waking hours.
Primary Headaches on One Page
A primary headache is defined as a headache without any other cause such as a tumor, a stroke, systemic diseases, etc. There are four categories of primary headaches, which are:
- Migraine
- Tension-type headache (TTH)
- Trigeminal Autonomic Cephalalgias (TACs)
- Other
The following are some crazy mnemonics that Dr. Hirschinger created as an easy way to teach orofacial residents how to remember the various criteria for the primary headaches. There are variations of these headaches but what follows below is the classical definition of each headache as defined by the International Headache Society criteria.
1. Migraine 5472 PUMA PPNV ACE
5472 = History of 5 headaches lasting between 4 and 72 hours
PUMA = at least 2 of 4: Pulsating, Unilateral, Moderate to severe, Aggravation with exertion or the avoidance thereof.
PPNV = at least 1 of 2 (1) Photophobia and Phonophobia (2) Nausea and/or Vomiting
ACE = remember to ask about Aura. Chronic = 15 or more headaches/month. Episodic = less than 15 headaches/month
2. Tension-type headache (TTH) 307 Almost the exact opposite of migraine
A. At least 10 episodes of headache occurring on an fulfilling criteria B-D:
Infrequent: <1 day/month on average (<12 days/year)
Frequent: At least 10 episodes of headache occurring on 1-14 days/month on average for >3 months (≥12 and <180 days/year)
Chronic: Headache occurring on ≥15 days/month on average for >3 months (≥180 days/year)
B. Lasting from 30 minutes to 7 days for infrequent and frequent. Chronic lasts hours to days, or is unremitting.
C. Headache has at least two of the following characteristics:
1. bilateral location
2. pressing/tightening (non-pulsating) quality
3. mild or moderate intensity
4. not aggravated by routine physical activity such as walking or climbing stairs
D. Both of the following:
1. no nausea or vomiting. Chronic can report mild nausea.
2. no more than one of photophobia or phonophobia
The gentle jaw is very effective in helping treat tension-type headaches.*

3. Trigeminal Autonomic Cephalalgias (TACs) Quarter to 3, 2:30, 1:10, greater than 3 months. The headache must be one sided and meet the criteria below:
3.1 Cluster: Quarter to 3 = 15 minutes to 3 hours. Must have an autonomic sign and/or restlessness/agitation.
3.2 Paroxysmal hemicrania: 2:30 = 2 minutes to 30 minutes. Must have an autonomic sign and/or restlessness/agitation.
*Responds absolutely to therapeutic doses of indomethacin.
3.3 SUNCT/SUNA: 1:10 = 1 second to 10 minutes. Must have an autonomic sign. SUNCT both conjunctival injection and lacrimation (tearing)*. SUNA only one or neither of conjunctival injection and lacrimation (tearing)*. *Ipsilateral to the pain.
3.4 Hemicrania continua: greater than 3 months Must have an autonomic sign and/or restlessness/agitation.
*Responds absolutely to therapeutic doses of indomethacin.
4. Other primary headache disorders – MRI is required.
“I was stabbed, I became numb, I coughed, I had exertional sex outside at a cold picnic, where I heard persistent thunder.”
4.1 Primary cough headache (headache due to coughing) = coughed
4.2 Primary exercise headache (headache occurs during exercise) = exertional
4.3 Primary headache associated with sexual activity (headache occurs at or before orgasm) = sex
4.4 Primary thunderclap headache = thunder
4.5 Cold stimulus headache (headache due to consuming something cold) = cold
4.6 External-pressure headache (headache due to hat, headband, goggles, ponytail, etc.) = outside
4.7 Primary stabbing headache (sharp stabs in temporal region lasting a few seconds) = stabbing
4.8 Nummular headache (headache in temporal region the size of a half dollar) = numb
4.9 Hypnic headache (headache occurs at the same time during sleep) = picnic
4.10 New daily-persistent headache (NDPH) (patients can recall time, day, and what they were doing when the headache started) = persistent
Here is a link to a downloadable PDF of the Primary Headaches on One Page, which you are free to share as long as the document remains unedited.
*Dr. Hirschinger is the inventor of the gentle jaw®, a passive stretching device for treatment of acute and chronic TMJ and muscle pain. gentle jaw is “yoga for the jaw®.”