Trigeminal neuralgia is considered one of the most painful conditions known to mankind. It is a sharp, shooting, electrical pain, which can mimic a toothache. This is because the trigeminal nerve innervates all of the teeth and their supporting structures such as the gum and the bone. The pain is generated from the brain but because of the way the nerve pathways work, patients will swear that the pain is from their tooth or from even multiple teeth. However, the pain will persist no matter what you do to treat the tooth including a crown, a root canal or even an extraction. Yes, even if a tooth is removed, the pain caused by trigeminal neuralgia will remain.
Diagnosis
The diagnosis of trigeminal neuralgia can sometimes be very simple. A well-trained clinician should never touch a tooth without having clear clinical and/or radiographic (x-ray) evidence of pathology such as decay, a tooth that is cracked, or symptoms based on hot and cold sensitivity and biting pressure. Additionally, tooth pain can throb and remain painful for hours and days. Trigeminal neuralgia only lasts a few seconds or minutes but the pain completely goes away, and it typically but not always does not bother patients during sleep.
Some patients have what we call a “trigger zone,” which is an area that can be pressed firmly or touched lightly with a Q-tip to trigger the pain. If a trigger zone is found, then the next step is to try to block the pain. The first step is to try to block trigeminal neuralgia with topical anesthetic placed directly on the trigger zone with a Q-tip. After waiting several minutes, the Q-tip test with pressure and light touch is repeated to see if the pain can be replicated. If it cannot, then it is likely trigeminal neuralgia since most dental pain cannot be blocked with topical anesthetic. If the pain cannot be blocked with topical, then the local tissue is numbed, and if that does not block the pain, then the tooth is numbed. If the pain is not blocked with any of these anesthetics, then the pain is likely centralized, and trigeminal neuralgia is likely ruled out. If the pain can be blocked, then it is likely trigeminal neuralgia but the patient will need an MRI to rule out space containing lesions such as a brain tumor, acoustic neuroma, multiple sclerosis, etc. The most important word to remember is “electrical.” If a patient ever describes electrical pain that completely resolves after a few seconds or a few minutes, then the pain is very likely due to trigeminal neuralgia.
MRI
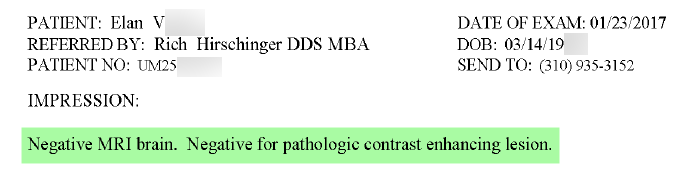
An MRI is absolutely required if the healthcare provider suspects trigeminal neuralgia. A physician or a dentist can order an MRI. The prescription I write for my patients in my Beverly Hills office for an MRI is usually:
High-resolution MRI with and without contrast of the brain and brain stem with thin cuts through the posterior cranial fossa with attention to the trigeminal nerve using Fiesta images with vascular loop protocol. Rule out space containing lesions, multiple sclerosis, acoustic neuroma, trigeminal neuralgia, etc. Please rule out contact of superior cerebellar and anterior inferior cerebellar arteries with the trigeminal nerve.
This image shows the MRI of a patient I was treating was normal.
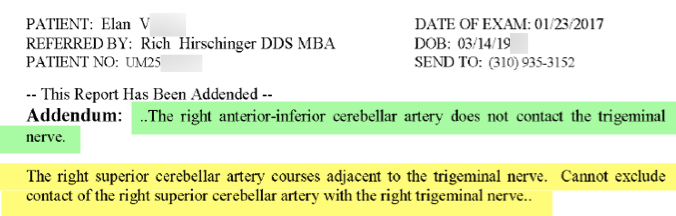
However, the radiologist did not address if one of the two arteries were in contact with the trigeminal nerve so a follow-up contact with the radiologist asked him to rule out that the arteries were not touching the trigeminal nerve. As you can read, the right superior cerebellar artery was likely in contact with the trigeminal nerve, which can account for the patient’s pain.
Treatment
After an MRI is obtained and is clear for space containing lesions, the patient has a couple of options depending on the results of the MRI. If the superior cerebellar artery or the anterior inferior cerebellar artery are in contact with the trigeminal nerve, the patient is treated using anti-seizure medications and/or they can consult with a neurosurgeon to learn about surgical options such as a microvascular decompression (MVD). If either of these arteries is not touching the nerve, then a neurosurgeon is not as likely to be successful with an MVD procedure. Typical anti-seizure medications include gabapentin, oxcarbazepine, carbamazepine, Lyrica, Keppra, Lamictal, etc.
If you have any questions about trigeminal neuralgia if you are a doctor or if you are a patient, or if you are interested in having me lecture to your group of any size, please feel free to contact me at my Beverly Hills office, which is 310.359.9080.